Weight loss surgery is one of many deadly health care industry frauds perpetrated on Americans. This blog was created to put a hurt on the greedy and criminal weight loss surgery industry and offer alternatives to the many many people who need to and want maintain a low and healthy body weight without the risk of death and permanent injury.
My Blog List
Tuesday, December 10, 2013
Warning to Spammers and Other Scum
We will refer you and the websites you promote to Anonymous. They know how to fuck with you fuckers.
Tuesday, November 12, 2013
Gastric Bypass Kills Readership
The only thing that the criminal medical industry understands is money and Gastric Bypass Kills is steering so many potential victims away from these butcher/surgeons that it is costing the weight loss surgery industry some serious money.
Nothing in today's medical industry is about patient/medical consumer welfare. It's almost always about the money.
Pageviews all time history 925,597
We encourage our readers to share this information with everyone everywhere. Feel free to cut and paste any and all information from this site. Post this information on weight loss and bariatric surgery forums. Help put this delporable industry out of business.
Nothing in today's medical industry is about patient/medical consumer welfare. It's almost always about the money.
Pageviews all time history 925,597
We encourage our readers to share this information with everyone everywhere. Feel free to cut and paste any and all information from this site. Post this information on weight loss and bariatric surgery forums. Help put this delporable industry out of business.
Wednesday, October 30, 2013
Obamacare Won't Cover Weight Loss Surgery
This is not a good thing since most fat people live in the South and most of them are Republicans. With 1 in 50 dying from he complications of weight loss surgery free weight loss surgery could wipe out enough fat Republicans to turn some Southern states like Texas and North Carolina into blue states.
JACKSON, Miss. — Uninsured Americans who are hoping the new health insurance law will give them access to weight loss treatments are likely to be disappointed. That’s especially the case in the Deep South where obesity rates are some of the highest in the nation, and states will not require health plans sold on the new online insurance marketplaces to cover medical weight loss treatments, whether prescription drugs or bariatric surgery.
Dr. Erin Cummins directs the bariatric surgery department at Central Mississippi Medical Center in the state capital of Jackson. She grew up in the Delta, her husband is a cotton farmer, and although she’s petite and fit, she understands well enough how Mississippians end up on her operating table.
You have to realize in the South, everything revolves around food. Reunions, funerals, parties — everything revolves around food,” Cummins says.
That long-standing culture – and other factors like inactivity and poverty – have saddled Mississippi with the highest obesity rate in the nation. Doctors here are no longer surprised to see 20-somethings with diabetes, hypertension, sleep apnea, heart disease and severe joint pain. And the prevalence of severe and super-obesity is growing rapidly. For those patients, bariatric surgery is considered the most effective treatment to induce significant weight loss.
Obamacare Insurance Won’t Cover Weight-Loss Surgery In Many States
JACKSON, Miss. — Uninsured Americans who are hoping the new health insurance law will give them access to weight loss treatments are likely to be disappointed. That’s especially the case in the Deep South where obesity rates are some of the highest in the nation, and states will not require health plans sold on the new online insurance marketplaces to cover medical weight loss treatments, whether prescription drugs or bariatric surgery.
Dr. Erin Cummins directs the bariatric surgery department at Central Mississippi Medical Center in the state capital of Jackson. She grew up in the Delta, her husband is a cotton farmer, and although she’s petite and fit, she understands well enough how Mississippians end up on her operating table.
You have to realize in the South, everything revolves around food. Reunions, funerals, parties — everything revolves around food,” Cummins says.
That long-standing culture – and other factors like inactivity and poverty – have saddled Mississippi with the highest obesity rate in the nation. Doctors here are no longer surprised to see 20-somethings with diabetes, hypertension, sleep apnea, heart disease and severe joint pain. And the prevalence of severe and super-obesity is growing rapidly. For those patients, bariatric surgery is considered the most effective treatment to induce significant weight loss.
Tuesday, September 3, 2013
The Statistical Truth About Gastric Bypass
Weight Gain After Short- and Long-Limb Gastric Bypass in Patients Followed for Longer Than 10 Years
Abstract
Objective:
To complete a long-term (>10 years) follow-up of patients undergoing isolated roux-en-Y gastric bypass for severe obesity.
Background:
Long-term results of gastric bypass in patients followed for longer than 10 years is not reported in the literature.
Methods:
Accurate
weights were recorded on 228 of 272 (83.8%) of patients at a mean of
11.4 years (range, 4.7–14.9 years) after surgery. Results were
documented on an individual basis for both long- and short-limb gastric
bypass and compared with results at the nadir BMI and % excess weight
loss (%EWL) at 5 years and >10 years post surgery.
Results:
There was a significant (P < 0.0001) increase in BMI in both morbidly obese (BMI < 50 kg/m2) and super obese patients (BMI > 50 kg/m2)
from the nadir to 5 years and from 5 to 10 years. The super obese lost
more rapidly from time zero and gained more rapidly after reaching the
lowest weight at approximately 2 years than the morbidly obese patients.
There was no difference in results between the long- and short-limb
operations. There was a significant increase in failures and decrease in
excellent results at 10 years when compared with 5 years. The failure
rate when all patients are followed for at least 10 years was 20.4% for
morbidly obese patients and 34.9% for super obese patients.
Conclusions:
The
gastric bypass limb length does not impact long-term weight loss.
Significant weight gain occurs continuously in patients after reaching
the nadir weight following gastric bypass. Despite this weight gain, the
long-term mortality remains low at 3.1%.
In
the past, we reported the results of gastric bypass in 274 patients
consecutively operated upon, who were followed for a mean of 5.5 ± 1.5
years (range, 3–8.4 years).1,2
We were concerned with weight loss and how this was influenced by
preoperative weight, time to follow-up, and the presence of a long- or
short-limb bypass. We emphasized clinical classification of all patients
as excellent, good, or failure on the basis of final body mass indices.3 We also compared our results of gastric bypass to those reported by Marceau et al4
with biliopancreatic diversion with duodenal switch because they,
uniquely, in the literature provided data on the above-mentioned
variables with a similar follow-up time.
It is the
purpose of the present study to report follow-up on the same patients
after a mean of 11.4 years (range, 4.7–14.9 years) and again to compare
the results to those achieved with biliopancreatic diversion and
duodenal switch with follow-up of all patients greater than 10 years.5
METHODS
Patient Follow-up
This
is a retrospective study in which patients were contacted by a
questionnaire and invited to return to our outpatient department for
examination, or provide the name of a local doctor to supply that
information, or depended on a phone conversation with the patient. The
study was conducted in accord with the ethical standards of the
Committee on Human Experimentation of the McGill University Health
Center. In the questionnaire, patients were asked to report on their
preoperative and postoperative health status and if they suffered from
any comorbidities of obesity or postoperative complications of gastric
bypass. The provincial health insurance system provided the addresses on
all patients, which is necessary to maintain a Medicare card (universal
health care system). In the cases where questionnaires were not
returned, addresses were cross referenced in a telephone directory
available on the Internet (http://www.canada411.ca),
after which patients were invited to our outpatient clinic or, if this
was not possible, were asked to provide information over the phone.
Weights obtained by questionnaire or telephone were compared with
weights revealed at the time of clinic visits. Deaths, time of death,
and cause were documented.
Operative Technique
All operations were performed by open laparotomy using a previously reported technique.1,2
Briefly, a small 4-cm-long pouch on the lesser curvature of the stomach
was created adjacent to a 28 or 30 Maloney bougie with a V. Mueller
PI-90 stapler (MMM Company, St. Paul, MN) using 4.8-mm staples. This
stapler is used to make 2 double rows of stables with an interval of
free tissue in between that permits division by sharp dissection or
cautery. The staple line of the pouch was oversewn with PDS sutures and
the staple line of the excluded gastric body was inverted. Omentum was
sutured between the staple lines. A proximal loop of jejunum was divided
10 cm from the ligament of Treitz and the distal end was advanced in a
retrocolic, retrogastric position to create a 40 cm Roux-en-Y limb,
which was anastomosed to the small gastric pouch. This was the operation
designated as the short-limb procedure (Fig. 1A).
The long-limb operation was created by dividing the jejunum 100 cm
distal to the ligament of Treitz and making the Roux-en-Y limb also100
cm (Fig. 1B).
The anastomosis had always enlarged to the diameter of the adjacent
jejunum when measured at endoscopy after 6 months to 1 year. This
enlargement occurred whether absorbable or nonabsorbable suture material
was used.
Outcomes Reporting
We used a modification of the Reinhold classification3 to evaluate our outcomes based on the body mass index (BMI) attained after 10 or more years of follow-up. (Table 1). An excellent or good result (BMI ≤ 35 kg/m2) was considered a success. We have also used the method of Biron et al5 to classify results after 10 years whereby success is achieved for morbidly obese patients if the BMI is <35 kg/m2 and for super obese <40 kg/m2.
We compared the results of the patients classified before surgery as
either morbidly obese or super obese over time and the influence during
that time of a long- or short-limb bypass.
Statistics
All
statistical analyses were performed using SPSS 12.0 for windows. All
mean BMIs in both morbid and super obese groups were tested for
significance using a one-way analysis of variance with posthoc testing
of the various means using Scheffé's test. The individual results at 5
and 10 years were tested for significance using the Pearson χ2
test. Change in BMI and estimated weight loss (%EWL) (preoperative
minus postoperative BMI or %EWL) was used to assess the magnitude of
weight loss between groups with different limb lengths using the
independent sample t test.
RESULTS
Of
the 272 consecutive patients in this series, 228 (83.8%) were followed
up. Of these, 76% were seen in our outpatient department or by their
local doctor and 24% provided information via questionnaire or a
telephone conversation. We asked 41 patients to provide us with their
weight by telephone prior to coming to the clinic in the next 2 to 3
days for complete follow-up including accurate weight measurements. We
found that 36 patients underestimated their actual weight by 5.8 ± 1.1
kg and 5 overestimated their actual weight by 3.8 ± 1.2 kg. Because of
this variability, we elected not to apply any correction factor to the
weight data reported by phone or questionnaire alone. A total of 161
patients were followed longer then 10 years, 60 patients were followed
for at least 5 years, 43 were lost to follow-up, 1 patient died within
30 days of surgery, and 7 patients died during the long term follow-up
period. The distribution of BMIs was as follows: 35 to 39, 6.3%; 40 to
49, 57%; 50 to 59, 29.8%; and >60, 7%.
One patient
died of pulmonary embolus on the second postoperative day for a 0.36%
30-day operative mortality. Seven patients died post surgery at: 4.8
years of suicide, 5.7 years of suicide, 6.6 years of liver failure, 8
years of unknown cause, 8.8 years of pulmonary embolus, 8.8 years of
cardiac failure, and at 13 years of cerebrovascular accident, for a 3.2%
long term post operative mortality.
Of the 272 patients in the study, 172 (63.2%) were morbidly obese (BMI < 50 kg/m2) and 100 (36.8%) were super obese (BMI ≥ 50 kg/m2).
A total of 189 (69.5%) had a short-limb operation and 83 (30.5%) had
the long-limb operation. We performed the short-limb operation up to the
end of 1993 and begun using the long-limb operation after that time
based on the popularity of adding more “malabsorption” to the short-limb
Roux-en-Y gastric bypass. Because of the numbers of patients operated
upon, the ratios of short- versus long-limb bypass remained relatively
consistent between the subgroups. Of the 172 morbidly obese patients,
119 (69%) had the short-limb operation and 53 (31%) had the long-limb
operation. Of the 100 super obese patients, 70 (70%) had the short-limb
operation and 30 (30%) had the long-limb operation.
The cumulative weight loss and characteristics of the patient population appear in Table 2.
The lowest BMI of the morbidly obese patients we were able to follow
was 26.4 and occurred at 1.9 years after surgery. This increased to 31.0
at final analysis 11.4 years after surgery. The lowest BMI for the
super obese patients we were able to follow was 31.4 and occurred at 2.2
years following operation. This increased to 38.3 at final evaluation
11.6 years after surgery. A similar pattern was seen with the %EWL.
Figure 2
shows the raw BMI data of all 228 patients at their last follow-up time
point. The mean follow-up period was 11.4 years. A number of patients
have BMI values above 35 and the majority are super obese patients with
starting BMI >50. The change in mean BMI over time for 161 patients
followed for more than 10 years appears in Figure 3. There is significant weight gain (P
< 0.0001) from the lowest BMI at approximately 2 years compared with
5 years after surgery and from 5 to 10 years after surgery in all
patients or when the patients are separated into morbidly obese (BMI
< 50) and super obese (BMI ≥ 50). Additionally, there is a
significant difference (P < 0.0001) between morbid obese and
super obese curves. The super obese lose more rapidly from the
preoperative BMI to the lowest BMI and gain more rapidly than the morbid
obese patients thereafter (P < 0.0001). Similar trends in
weight regain when patients are followed more then 10 years are shown
when the %EWL is examined (Fig. 4).
The best %EWL was 89%, observed at about 2.5 years post surgery and
decreased significantly to 68.1% at about 12.3 years post surgery (P < 0.001).

FIGURE 2.
Plot of raw BMI values of 228 patients post RY gastric bypass at the
last follow-up period (11.4 ± 2.8 years, mean ± SD) stratified by BMI
into morbid obesity (BMI < 50) and superobesity (BMI ≥ 50).

FIGURE 3.
Plot of decrease of BMI against time for the 161 patients followed for
more then 10 years (up to 15). The points represent the mean ± SD. Point
0 is the preoperative BMI. The nadir or lowest BMI occurred at 2.2 ±
1.9 years. The ...

FIGURE 4.
Plot of % excess weight loss against time for the 161 patients followed
for more then 10 years (up to 15). A significant weight regain occurs
following the best weight loss at about 2.5 ± 2.1 years compared with
longer follow-up periods ...
The individual results based on the Reinhold classification appear in Table 3.
There is a significant decrease in excellent results and increase in
failures from the results obtained within the first 5 years of follow-up
compared with those obtained after more then 10 years of follow-up in
all patients or when stratified by BMI into morbid obesity or super
obesity.
TABLE 3.
Gastric Bypass Results for Severe Obesity According to the Reinhold
Classification for Patients That Were Followed for 10 or More Years
(Maximum 15 Years)
While the long-limb bypass appears to improve the results slightly at 5 years in the super obese patients (Fig. 5),
this difference was not significant. Furthermore, this apparent benefit
was no longer seen at 10 years of follow-up. In patients who had a BMI
over 60 kg/m2, who might be benefited by the long-limb
operation the most, the final BMI was 37.8 ± 4.4 in long-limb patients
and 42.9 ± 9.6 (mean ± SD) in the short-limb group, but this difference
is not significant (P = 0.133). Table 4
shows the detailed analysis of the effect of limb length on long-term
weight in morbidly obese or superobese patients. Because of the
sequential study design, the follow-up was significantly shorter in the
long-limb group. However, neither change in BMI nor final BMI was
different between the short- and long-limb groups, even when the
patients are stratified by BMI to morbidly obese and super obese groups.

FIGURE 5. The effect of limb length on long-term weight loss in morbidly obese (MO) and super (MO) obese patients.
A comparison of failure rates in the biliopancreatic diversion with duodenal switch operation reported by Biron et al5 and the gastric bypass as performed at our center appears in Table 5. All patients in both groups were followed over 10 years after surgery. We compared failure rates based on final BMI ≥35 kg/m2 for morbidly obese and BMI ≥40 kg/m2
for super obese patients. The 2 different operations produce comparable
failure rates in patients who are followed for more then 10 years post
surgery according to their criteria.
DISCUSSION
Significant
weight gain after gastric bypass just like the results reported after
biliopancreatic diversion with duodenal switch is a prominent feature of
this retrospective study. The modest lengthening of the Roux and
afferent limbs in the gastric bypass operation did not improve weight
loss when comparisons are made after 10 years of follow-up. One could
dispute the definition of success herein defined. We agree with Biron et
al5 that patient satisfaction is low when morbidly obese patients have a final BMI >35 kg/m2 and when super obese patients have a final BMI >40 kg/m2 many years after their operation.
Other long-term studies (>10-year follow-up) do not confirm the late failure rates herein reported. Hess et al6 were able to follow 167 of 182 patients (92%) more than 10 years after biliopancreatic diversion with duodenal switch. They found 87 (52%) had lost at least 80% of excess weight. Only 6% lost less than 50% of excess weight.6 We found that 55 of 161 (34%) of our patients had lost at least 80% of excess weight after more than 10 years follow-up. Hess et al report a mean initial excess weight loss of 75% (no SD reported) for patients followed for more then 10 years.6 This compares with 68.6% ± 21.4% (mean ± SD) reported by Biron et al5 and 67.6% ± 25.1% (mean ± SD) reported herein for the gastric bypass operation.
Scopinaro et al7
have reported excess weight loss of 74% ± 15% (mean ± SD) at 10 years,
75% ± 16% at 12 years, 75% ± 16% at 14 years, and 77% ± 18% at 18 years
with no difference between morbid obese and super obese patients. At 10
years, 90% of the patients had a reduction of the initial excess weight
>50%. In our case, 80% of our patients had a reduction of the initial
excess weight >50%.
Fobi et al8 using the transected banded gastric bypass followed 22 of 51 patients for 10 years and reported a mean of 72% excess weight loss, but no range (eg, mean ± SD) of results or stratification based on preoperative weight was supplied. Their data are similar to ours with 67.6% excess weight loss at >10 years follow-up.
Pories et al9 showed a remarkable stability of postoperative weight after gastric bypass for up to 14 years. Their study of 608 patients with a 97% follow-up showed a 58% loss of excess weight after 5 years and a BMI of 33.7. After 10 years, the excess weight loss was 55% and the BMI was 34.7 (range, 22.5–64.7). At 14 years (10 patients), the EWL was 49% and the BMI 34.9 (range, 25.9–54.6). Since only 158 of the 608 patients in this series were followed for 10 years, late weight gain may be missed.
Others have noticed weight gain from the nadir weight after gastric bypass. Ponce and Dixon10
found a decrease in excess weight loss at 5 to 7 years after gastric
bypass so that there was an overlap of this value between lap band
operations and gastric bypass.
The stratification of
severely obese patients into morbidly obese if the BMI is less then 50
and super obese when the BMI is greater or equal to 50 has not shown any
advantage in interpreting our outcome results after 10 years of
follow-up and the effect of limb length on this outcome. Up to the end
of 1994, which is the closing date for this study, 9.9% of patients had
BMI >60 with a maximum BMI = 80 (range, 35–80). The mean BMI of
patients that we see today has increased by at least 5 points and 15.4%
of the patients have BMI >60 with a maximum BMI = 105.5 (range,
35–105.5). Setting a BMI cutoff of 50 to stratify patients as super
obese ignores this trend and nullifies any recommendations. A better
stratification might be to report BMI centiles (10 BMI units) and use
this stratification to bring out the challenges of achieving weight loss
in these massive patients. Other variables such as race (eg, blacks
demonstrate less weight loss with bariatric surgery compared with
whites) or perhaps genetic profiles may also have to be considered.
Despite
significant weight gain, which does impact on quality of life as judged
by the patients, the mortality rate has remained very low at 3.1% and
comorbidities have remained extremely low as judged by assessing the
medications the patients are currently taking. A larger study with
longer follow-up will be necessary to establish the impact of late
weight gain on recurrence of comorbidities.
Satiety is a
prominent feature of weight loss after gastric bypass and persists in
those patients with an excellent result. Patients who regain large
amounts of weight say they are eating almost as much as before the
operation. This increase in intake takes place over several years and
does not occur suddenly as with staple line dehiscence.
In
the past, we found that excellent weight loss occurred with a wide open
gastrojejunal anastomosis. We also did not show increase in pouch size
over a 5-year period using upper gastrointestinal x-ray examinations.
How satiety is controlled is not apparent from this study, but it is
quite clear that significant weight gain can occur in cooperative,
well-motivated patients who have experienced substantial improvement in
quality of life after surgery before late weight gain.
It
is equally puzzling that a malabsorptive procedure, the biliopancreatic
diversion with duodenal switch, should have a similar reported late
failure rate as a restrictive operation, the Roux-en-Y gastric bypass. A
prospective randomized trial comparing the 2 techniques with
appropriate follow-up periods (>10 years) is needed to confirm the
findings suggested by these retrospective studies.
Footnotes
Supported in part from an unrestricted education grant from Johnson & Johnson and by the LD MacLean Scholarship Fund.
Reprints:
Nicolas V. Christou, MD, PhD, Section of Bariatric Surgery, McGill
University Health Center, 687 Pine Ave. W., Montreal, Quebec, Canada H3A
1A1. E-mail: Nicolas.Christou@MUHC.McGill.ca.
REFERENCES
1. MacLean LD, Rhode BM, Nohr CW. Late outcome of isolated gastric bypass. Ann Surg. 2000;231:524–528. [PMC free article] [PubMed]
2. MacLean LD, Rhode BM, Nohr CW. Long- or short-limb gastric bypass? J Gastrointest Surg. 2001;5:525–530. [PubMed]
3. Reinhold RB. Critical analysis of long-term weight loss following gastric bypass. Surg Gynecol Obstet. 1982;155:385–394. [PubMed]
4. Marceau P, Hould FS, Simard S, et al. Biliopancreatic diversion with duodenal switch. World J Surg. 1998;22:947–954. [PubMed]
5. Biron S, Hould FS, Lebel S, et al. Twenty years of biliopancreatic diversion: what is the goal of the surgery? Obes Surg. 2004;14:160–164. [PubMed]
6. Hess DS, Hess DW, Oakley RS. The biliopancreatic diversion with the duodenal switch: results beyond 10 years. Obes Surg. 2005;14:408–416. [PubMed]
7. Scopinaro N, Marinari G, Camerini G, et al. Biliopancreatic diversion for obesity: state of the art. Surg Obes. 2005;1:317–328. [PubMed]
8. Fobi MA, Lee H, Felahy B, et al. Choosing an operation for weight control, and the transected banded gastric bypass. Obes Surg. 2005;15:114–121. [PubMed]
9. Pories
WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An
operation proves to be the most effective therapy for adult-onset
diabetes mellitus. Ann Surg. 1995;222:339–352. [PMC free article] [PubMed]
10. Ponce J, Dixon JB. Laparoscopic adjustable gastric banding. Surg Obes. 2005;1:310–316. [PubMed]
Monday, July 1, 2013
Worldwide Obesity Rate Is Growing As Fast as Your Surgeon's Wallet
The outlook is grim bright. The World Health Organization estimates that 1.6 billion people worldwide are overweight or obese. The death toll associated with obesity runs to 2.5 million annually, and the numbers haven’t reached their peak. The British Heart Foundation predicts that half the population of the UK could be obese within 25 years. The toll on health and quality of life is enormous. So is the price tag. A 2007 UK report estimated an annual loss in healthcare costs and lost working hours at £45billion (about US$72 billion.
Keep eating!
Keep eating!
Wednesday, June 26, 2013
Urea Cycle Failure Triggered by Gastric Bypass Surgery
This is another way gastric bypass can kill you. Urea cycle failure is a not so rare genetic disorder. It is also called wasting syndrome. As you may know gastric bypass works by bypassing nearly all the the small intestine. Shortening the small intestine causes an irreversible condition called mal-absorption syndrome. Mal-absortption makes the absorption of essential nutrients impossible.
Lying scumbag doctors told Hilary X that gastric bypass surgery was her option. None of them warned her knew about a
disorder called acquired urea cycle failure. As a result Hilary X died a prolonged and agonizing death.
Her problems began about four years after the gastric bypass surgery. Doctors at Vanderbilt University Medical Center were too stupid and too lazy to figure out what was killing her. No nutritional equation worked because her body was turning protein into ammonia and her liver was failing to convert it to urea. Her body could not excrete the toxin.
Her problems began about four years after the gastric bypass surgery. Doctors at Vanderbilt University Medical Center were too stupid and too lazy to figure out what was killing her. No nutritional equation worked because her body was turning protein into ammonia and her liver was failing to convert it to urea. Her body could not excrete the toxin.
Cynthia Le Mons, executive director of the
National Urea Cycle Disorders Foundation, believes the complication that
led to Hilary X's death is not as rare as doctors think. She knows
of six women who have developed urea cycle failure after gastric bypass
surgery since 2007. Five of the six died.
"That's just the tip of the iceberg," Le Mons said. "If we know about it, it's just a microcosm of what is going on."
Read more about how greedy butcher doctors killed Hilary Lane.
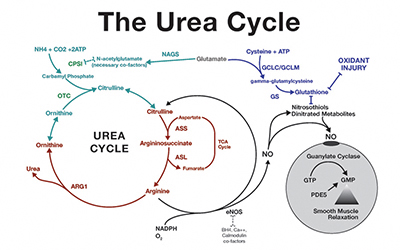 |
| A Biologist or an Engineer Can Understand This Most Doctors Can't! Doctor's Are Not All That Bright |
L-citrulline is a non-essential amino acid. In hepatocytes, the addition of carbon dioxide and ammonia to ornithine synthesizes L-citrulline during the urea cycle. The enzymes argininosuccinate synthetase and argininosuccinate lyase, when in the presence of L-aspartate and ATP, converts L-citrulline into L-arginine . Subsequently, L-arginine is converted to nitric oxide by nitric oxide synthase and L-citrulline is regenerated as a by-product .
Citrulline, a non-standard amino acid not normally present in protein, is an intermediate in the conversion of the amino acid ornithine to arginine during the urea cycle.
Citrulline Uses
Citrulline’s main function is its ability to remove ammonia and is essential for the excretion of oxidative waste processes. It is also used for treatment of Ornithine Transcarbamylase, a urea cycle disorder. Urea cycle disorder is a genetic disorder consisting of a deficiency of one of the enzymes needed in the urea cycle. Citrulline is critical in the improvement of immune system deficiencies and overall functioning.
Malic Acid, a key component of the energy production yielded via the Kreb’s cycle, conditions and assists lactate and pyruvate toward anabolism rather than catabolism. Supplementation of this nonessential amino acid has reduced fatigue significantly as well as increase energy production. Documentation has shown citrulline to significantly increase the body’s metabolic rate, aerobic performance, and provide reductions in the onset of muscular fatigue.
In conclusion, citrulline supplementation may not only boost physical activity performance, but also provide our bodies with a means of eliminating the amino acid breakdown products of protein metabolism. Equally important is the detoxification of ammonium and lactate from the blood.
Friday, May 3, 2013
Gastric Bypass Surgeons: Take Notice
103,784 vistors have visited Gastric Bypass Kills as of 5/3/16. Many of them are considering your deadly surgery and many others are family members of your victims.
There is no amount of money you bastards can give me that will make me take this site down.
By next year this time Gastric Bypass Kills with have over 300,000 visitors. Gastric Bypass Kills got 7000 page views today. I know that this site is putting a hurt on your business.
http://www.drmcdougall.com/forums/viewtopic.php?f=1&t=29453
Update: As of 6/617 1,882,678 people have visited Gastric Bypass Kills. We know that we are putting hurt on you greedy butchers.
BUT THIS IS WORSE!

There is no amount of money you bastards can give me that will make me take this site down.
By next year this time Gastric Bypass Kills with have over 300,000 visitors. Gastric Bypass Kills got 7000 page views today. I know that this site is putting a hurt on your business.
http://www.drmcdougall.com/forums/viewtopic.php?f=1&t=29453
 |
| Infected antibiotic resistant gastric bypass wound |
BUT THIS IS WORSE!

Saturday, April 13, 2013
Weight Loss Surgery Nightmare or Glutton's Dream?
Woman Now Has to Eat 5,000 Calories a Day to Stay Alive After Weight Loss Surgery
- Julie Dunbar, 51, had weight loss surgery after her weight hit 20st 7lb or 287 pounds.
- Lost 14 stone or 238 pounds in a year and became dangerously malnourished
- Needed tube feeding and three more ops to partly undo stomach reduction
- Now has illness resulting from severe malnourishment and lack of vitamins
- Has to eat 5,000 calories a day to get enough nutrients to stay alive
One of the drawbacks of gluttony is getting fat and obese. The whole point of life for fat people/gluttons is eating and the more we eat the happier we are. With this type of surgery gluttony no longer harm our health! How great is that!
By Chris Brooke
A pub landlady who underwent a gastric bypass operation has become so thin she must eat a mountain of food every day to stay alive.
The slimming surgery caused Julie Dunbar’s body to stop absorbing the nutrients it needs.
In 12 months, her weight plummeted from 20st 7lbs or 238 pounds to a skeletal 6st –84 pounds and she ended up in hospital dangerously malnourished and close to death.
 |
Full-time job: Ms Dubar says her daily calorie requirement (pictured) means she is 'constantly eating' and spends at least £200/$307 dollars a week on food.
Doctors told her the only solution was to eat 5,000 calories a day – more than double the recommended daily amount for women and far more than she ever used to eat – because her body can ingest only a fraction of the nutrients she takes in.
More...
- Father who lost 13 stone after gastric bypass surgery describes the agony of being left with TWO STONE of excess skin that hangs to his knees
- Fat people live longer 'because their brains get more nourishment under stress', says obesity doctor
- It CAN be too late: Obese people who only lose weight later in life may find their hearts irreparably damaged
Miss Dunbar, 51, of Leeds, West Yorkshire, said: ‘It’s a full-time job. Our food bill is phenomenal. It must cost about £200/$307 to feed me a week.
‘It was enjoyable at first
 |
| Plump and Pretty Sexy Sow Julie Dunbar Enjoying a Smoke |


In 2010, Miss Dunbar paid £10,000 to have the biliopancreatic diversion with a duodenal switch operation at the private Spire Hospital in Leeds. In this type of weight-loss surgery a large part of the stomach is removed and the small intestine re-routed. The object is to reduce the amount of time the body has to capture calories and absorb fat.
Following the operation, her weight dropped so quickly and her eating increased that her sister Karen, 50, was inspired to have the same procedure.
But while the sister’s weight levelled off at 10st, Miss Dunbar’s continued to drop at an
She said: ‘It was an absolutely
READ MORE HERE:
http://www.dailymail.co.uk/health/article-2288359/My-gastric-bypass-nearly-killed-Woman-eat-5-000-calories-day-stay-alive.html
Friday, April 12, 2013
The Truth About Healthcare In America
The criminal corporate thugs who run the American healthcare system would like you to believe that the reason healthcare is so expensive in the United States is because it is your fault. Criminals who run the American healthcare system are the same criminals who run the health insurance companies, drug companies, medical device companies and doctors.
Is not your fault that Americans pay three times the world average for healthcare. The American healthcare system is run by vile contemptible treasonous criminal corporatists.
Obesity in the short term does cost the health care system more but in the long term because fat people die sooner obesity actually cost the healthcare system less.
For any Obama haters reading this, you now have my permission for go fuck yourselves.
Tuesday, April 2, 2013
Bariatric Surgeons Are Incompetent
From Obesity Help
Gastric Bypass, and the surgeons who perform it, have left me near death, with a feeding tube, living off disability and uninsurable. That's why I need to share my story to explain some of the common, yet avoidable, complications of Bariatric Surgery. This surgery is becoming too commercialized and routine, and many times it's being performed without the patient being educated of the life-long changes they need to make in order to be successful and healthy long-term.
I had Bariatric Surgery, or Open Gastric Bypass, in December 2002. I was 33 years old and had been overweight and/or obese the majority of those years. I did at least 2 years of research before surgery plus continued my research post-op and was extremely excited for what was to come. Within the first two weeks I lost 18 pounds. Wow! Then it stopped. I was eating tiny, well-balanced 2 ounce meals but the weight would not budge. I did not touch sugar, fat or anything with high calories. I only drank water. I followed the doctors orders to the letter. But I was not exercising.
I started exercising and the weight started coming off. I exercised for 90 minutes, 6 days a week. If I stopped exercising for a week, it would take me a month to lose another pound. I fought for every pound I lost. It took two years, but at 5 feet, 3 inches tall, I went from 275 pounds to 160 pounds and was on top of the world, still exercising and eating right.
In March of 2008 I had some dental work done. I was put on 1600mg of ibuprofen a day for 2 months. Roughly 2 months after I discontinued the use of ibuprofen I started vomiting. It quickly became a daily occurrence. One day after eating my small breakfast and lunch, around 2:00 PM I had to vomit again, but this time I realized it included dinner from the previous night.
Scared, I ended up at a gastroenterologist who ran a camera scope down my throat and said that the opening from my stomach to my intestines had closed down to the size of a pinhole due to scar tissue. I was told that scar tissue is considered a common complication for Gastric Bypass patients. After reviewing my medical history he asked if I use ibuprofen, and I was then told that Gastric Bypass patients should not take ibuprofen or any NSAIDS, as it causes scar tissue. For 6 years I had been taking a few NSAIDS for aches and pains here and there. None of my doctors had said anything.
I wish my story ended there. To make this short, my gastroenterologist did a scope with balloon dilation to open up the scar tissue, a procedure that works on all but 2% of bypass patients. I am part of that 2%. After having 2 scopes with balloon dilation, I was told I needed Gastric Revision surgery.
On January 29, 2009 my new bariatric surgeon performed an Open Gastric Revision surgery, which split me from the tip of my chest-bone down to my belly button. He was well-known, recommended and even had a commercial on television about gastric bypass. However, right after surgery I was still vomiting. Not even two weeks after surgery they performed another scope down my throat and my gastroenterologist wrote in my record that the bariatric surgeon had sewn my stomach shut. Now, instead of a stricture from my stomach to my intestines, I had a stricture from my esophagus to my stomach. The surgeon denied it, saying that I had rebuilt scar tissue within those two weeks. After 5 months, 7 additional scopes with balloon dilation and 59 days in the hospital, I was forced to get a feeding tube, fired from my job, left with no insurance, and had to go on disability. I am now down to 121 pounds. I've lost all muscle mass, fat, menstruation, and nearly all of my teeth due to malnutrition. My nutrients are fed to me 12-16 hours a day through a tube in my chest that sits right on my bra line.
There is more to my story, but I tried to condense it as best as I could. I am trying to get my story to other patients, or those considering gastric bypass, through talk shows, magazines, online, etc., in hopes that by hearing my story I can help people realize that gastric bypass is not a quick fix. It's a tool, which if used correctly, takes effort, changes in diet, changes in medication and supplements, amount of food eaten and exercise. Things that can also be done without the surgery and some of the common complications that come with it. I'm hoping that patients and their doctors research and educate all facets of this procedure, short and long-term. I would not be where I am today if I had known NSAIDS caused scar tissue, and I have researched this surgery extensively. I'm also hoping that by getting my story publicized, I might find a doctor who specializes in this field as I'm told I need additional surgery to make a new stomach out of my remaining intestines. Until then, I will survive on my feeding tube and disability.
I appreciate you reading my story. I hope this is not the end of my story, but just a positive beginning. Thank you so much for your time.
Leslee
Reno, Nevada
Read More Gastric Bypass Horror Stories Here!
More deaths from Gastric Bypass video, this could save your life!
Sunday, March 24, 2013
Corrupt FDA Corrupt Doctors
Americans Fed up with Drug Industry Influence and FDA Corruption
By Mike
Adams, Natural News Editor
More than four out of five Americans think drug companies have
too much influence over the Food and Drug Administration, and 84 percent believe
that advertisements for prescription drugs with safety concerns should be
outlawed, reveals a striking new survey from Consumer Reports.
The survey results, released today, are based on a telephone survey of 1,026 American adults conducted by the Consumer Reports National Research Center. They reveal the Food and Drug Administration to be alarmingly out of touch with the concerns of the American people. Some of the most interesting results include:
• 96 percent agreed the government should have the power to require warning labels on drugs with known safety problems. As Consumer Reports explains, "Right now, the Food and Drug Administration must negotiate safety warning labels with a drug maker."
• 84 percent agree that drug companies have "too much influence over the government officials who regulate them." More than two-thirds of those surveyed are concerned that drug companies actually pay the FDA to review and approve their drugs. It's a situation that turns drug companies into the "customers" of the FDA. (See related cartoon, The Puppets of Big Pharma)
• 92 percent agree that pharmaceutical companies should disclose the results of ALL clinical trials, not just the ones with positive results that they wish to publicize. (Currently, drug companies can bury negative drug trials, and the FDA has in fact been caught conspiring with drug companies to keep negative drug data secret from the public.)
• 93 percent think that the FDA should have the power to demand follow-up
safety studies from drug companies. Currently, the FDA has no authority to
require follow-up safety studies on drugs after they are introdued to the
market. This is a serious oversight shortfall, given that many problems with
drugs only appear after widespread use. (Patients are widely used as guinea pigs
in any new drug launch.)The survey results, released today, are based on a telephone survey of 1,026 American adults conducted by the Consumer Reports National Research Center. They reveal the Food and Drug Administration to be alarmingly out of touch with the concerns of the American people. Some of the most interesting results include:
• 96 percent agreed the government should have the power to require warning labels on drugs with known safety problems. As Consumer Reports explains, "Right now, the Food and Drug Administration must negotiate safety warning labels with a drug maker."
• 84 percent agree that drug companies have "too much influence over the government officials who regulate them." More than two-thirds of those surveyed are concerned that drug companies actually pay the FDA to review and approve their drugs. It's a situation that turns drug companies into the "customers" of the FDA. (See related cartoon, The Puppets of Big Pharma)
• 92 percent agree that pharmaceutical companies should disclose the results of ALL clinical trials, not just the ones with positive results that they wish to publicize. (Currently, drug companies can bury negative drug trials, and the FDA has in fact been caught conspiring with drug companies to keep negative drug data secret from the public.)
 FDA Conflicts of Interest. Click to view full cartoon. |
New rules proposed by the FDA would reduce this level of corruption by allowing doctors to receive a maximum of $50,000 per year from companies impacted by their decisions. (Thereby making the FDA numerically less corrupt than it is now, but still tolerating blatant conflicts of interest. It's like setting a "bribery ceiling.")
• 91 percent said they had seen a drug advertisement on television or in print (a "victory" accomplished by the FDA legalizing such ads in 1998), and 26 percent said they asked their doctor for a brand-name medication after learning about it from an advertisement. This is the purpose of advertising, of course: To increase sales of drugs, not -- as is claimed by Big Pharma and the FDA -- to "educate" patients about medical treatments.
• 75 percent agreed that the allowing of drug advertising has resulted in the over-prescribing of pharmaceuticals. Fifty-nine percent said the government should restrict pharmaceutical advertising, and 26 percent said they "strongly agree" with such restrictions.
Direct-to-consumer advertising is the bread and butter of Big Pharma, and it is the primary reason the industry has exploded its revenues and influence since 1998. The invention and marketing of fictitious diseases via television advertising has proven instrumental to the drug industry's successful pushing of medically unjustified drugs onto consumers. (See the Disease Mongering Engine to invent your own fictitious diseases and disorders right now!)
• The survey further revealed 54 percent of consumers think that viewing drug advertisements allows them to "take charge of their health care." The survey did not, however, reveal whether these people were in fact suffering from deterimental cognitive side effects at the moment they were taking the survey. Statistically, it seems reasonable to assume that approximately half of the adults taking the survey were on drugs at the time they were answering the survey questions.
 When Pharmacists Tell the Truth. Click to view full cartoon. |
Most side effects go unreported, and there is currently no enforced legal requirement that doctors or drug companies report known side effects to the FDA. According to the Journal of the American Medical Association, prescription drugs currently kill approximately 100,000 Americans each year. None of those deaths are accurately recorded as "death by pharmaceuticals."
• As mentioned earlier, 84 percent agree that advertisements should be outlawed for drugs with safety concerns. The United States is the only advanced nation in the world that allows drug companies to advertise directly to consumers. It was legalized in 1998 by the FDA, following political pressure and influence from the drug companies who knew that being able to promote fictitious diseases and push brand-name drugs would result in windfall profits. (Some drugs are sold at markups as high as 300,000% over the cost of their ingredients.)
The makers of Vioxx and Paxil had studies that indicated safety problems for years, but did not release those results to the public. - Consumer Reports The real threat of pharmaceuticals
Interestingly, the survey did not ask consumers the following question: How many Americans do you think is acceptable for the drug companies to kill each year?
Because right now, that number is, conservatively, about 100,000 American citizens. More realistic estimates put it at double that number, or 200,000. I've often stated that pharmaceuticals kill more Americans each year than diet in the entire Vietnam War, and the number of Americans killed by acts of terrorism are dwarfed by the number killed by prescription drugs that the FDA and drug companies unquestionably knew were killing people. It's not that these deaths were truly accidental... they were fully documented but ignored anyway by an industry that is now clearly a very real threat to the health and safety of the American people.
This is no exaggeration: The number of people killed by FDA-approved pharmaceuticals since 9/11 is equivalent to dropping a nuclear bomb on a major U.S. city. International terrorists could not even hope to cause the number of casualties in the United States that have been achieved by the drug companies working in conspiracy with the FDA.
If we don't put limits on the influence and corruption of the drug companies by banning drug ads and demanding serious FDA reforms, the body count will only get worse. Consumers are finally waking up to this reality, and they're increasingly demanding "get tough" solutions that would require the FDA to protect the people instead of protecting Big Pharma profits.
As Bill Baughan, a senior policy analyst with Consumers Union (Consumer Reports), said, "Consumers expect Congress to take their concerns about drug safety seriously, and deliver legislation that will prevent future Vioxx-type disasters. Failure to act this year on the strongest possible bill, when more than 80 pecent of Americans agree that Congress should do whatever is necessary to ensure drug safety, would equate to gross legislative malpractice." Most Americans agree with NaturalNews
What's really interesting about these results is that they show most Americans agree with NaturalNews on issues like drug advertising, ending conflicts of interest at the FDA, requiring all clinical trials to be published, and other similar topics covered in this survey.
Meanwhile, very few Americans agree with the FDA or the wishes of organizations like the American Medical Association and drug companies themselves -- most of which like things just fine the way they are.
Drug companies, of course, would love to maintain the status quo and continue conducting business as usual. But thanks to grassroots consumer advocacy campaigns such as StopDrugAds (www.StopDrugAds.org), and sites like this one, the real story about the dangers of pharmaceuticals are no longer being censored and kept from the public.
The word is out: Pharmaceuticals are now the 4th leading cause of death in America. The best way to protect Americans from these dangerous, deadly products is to enact sweeping reforms that end the medical racket currently being operated by the FDA / Big Pharma tag-team.
Unfortunately, many of the very lawmakers who will vote on this pending legislation are, much like FDA advisors, "on the take" from the very same pharmaeutical companies that stand to be impacted by their vote. And no lawmakers that I know of are abstaining from the vote due to conflicts of interest. The reality is that Big Pharma has bought Congress, and whatever vote that will soon emerge is a far cry from the real reforms we'd see if our national lawmakers weren't financially beholden to the drug companies for their own reelection campaigns.
Thus, if Congress actually manages to pass a law that would eliminate drug company influence over FDA decision makers, it would be a clear case of lawmakers under the influence of drug money passing laws to eliminate the influence of drug money for others, but not for themselves.
There should be a law against that, it seems.
 The FDA Vision Test. Click to view full cartoon. |
True facts about the FDA
The following are facts about the FDA I've documented in my new book, Natural Health Solutions and the Conspiracy to Keep You From Knowing About Them. As this book reveals, the FDA has:| Worked to keep deadly drugs on the market as long as possible before
reluctantly pulling them (usually only after being sued by groups like
Public Citizen). The astonishing story of Rezulin, a diabetes drug, is a
good example. | |
| Repeatedly banned and confiscated herbs and nutritional supplements that
compete with prescription drugs. Ephedra, for example, was banned by the FDA
based on a political agenda, not good science. | |
| Conducted armed raids on alternative medicine clinics, confiscating
computers, threatening alternative health practitioners, and scaring away
patients. (See Tyranny in
the USA: The true history of FDA raids on healers, vitamin shops and
supplement companies) | |
| Ordered the destruction of recipe books promoting stevia, a natural
sweetener that competes with sales of aspartame
(yes, the FDA actually ordered the books to be destroyed). | |
| Been caught red-handed accepting bribes. | |
| Voted to put deadly drugs right back on the market even after such drugs
were recalled by their manufacturer. | |
| Openly opposed the banning of junk food
advertising to children during World
Health Organization meetings. | |
| Suppressed information about the harm caused by dangerous
drugs in order to prevent the press and the public from learning
the truth about them. | |
| Attempted to silence its own drug safety scientists to prevent them from
going public with the truth about dangerous drugs. | |
| Censored scientific information about the benefits of natural foods like cherries
by threatening cherry growers with legal action if they did not remove
scientific information about cherries from their websites. (See FDA
tyranny and the censorship of cherry health facts) | |
| Pursued and shut down companies selling genuine cancer
cures that provably work better than any prescription
drug (such as Lane Labs' MGN-3). | |
| Vigorously argued against making "optimal health" a goal of the
Codex Alimentarius discussions, striking the phrase from the final report. | |
| Rigged its drug safety review panels with decision makers who have
substantial financial ties to drug companies, even while refusing to
disclose such blatant conflicts of interest. | |
| Planned, organized, and took part in armed "SWAT-style" raids on
vitamin shops, pet food stores, and even a church. | |
| Knowingly approved harmful food
additives for widespread use in the
food supply (such as aspartame, which has a rather dubious history and
has been proven toxic in several studies), even when its own safety experts
recommended denying approval. | |
| Allowed the continued legal use of harmful, cancer-causing food additives
in the national food supply such as sodium nitrite (which causes cancer and
yet is intentionally added to nearly all processed meats). | |
| Refused to ban a poisonous artificial fat from the food supply (hydrogenated
oils) for decades, even though the World Health Organization urged
member nations to outlaw the substance in 1978. Hydrogenated oils continue
to harm infants, children, and adults today. |
It is clearly time to reform not merely the FDA, but the entire medical industry. Drug companies are running amok, and this new Consumer Reports survey reveals that consumers are finally fed up with it.
Saturday, March 23, 2013
Another Reason to Avoid Weight Loss Surgery
Click HERE to watch the Full Interview!
Download Interview Transcript
Download Interview Transcript
Visit the Mercola Video Library
By Dr. Mercola
Medical errors are one of the leading causes of death in the United States, and what’s even more shocking is that the harm often is preventable.
Hospitals often make egregious errors ranging from minor mistakes to treating the wrong patient, leaving behind surgical tools in a person after surgery, or operating on the wrong body part.
According to the 2011 Health Grades report,1 the incidence rate of medical harm occurring in the United States is estimated to be over 40,000 harmful and/or lethal errors DAILY!
Dr. Martin Makary is the author of The New York Times bestselling book Unaccountable: What Hospitals Won’t Tell You and How Transparency Can Revolutionize Healthcare, which is a story about the dangerous practices and mistakes of modern medicine. He’s a practicing surgeon at Johns Hopkins Hospital and an associate professor of public health policy at the Johns Hopkins School of Public Health.
As a busy surgeon, he’s worked in many of the best hospitals in the country, and can testify to the amazing power of modern medicine to cure. But he’s also been a witness to the medical culture that routinely leaves surgical sponges inside patients, amputates the wrong limbs, and overdoses children because of sloppy handwriting.
Healthy eating, exercise, and stress management can help keep you OUT of the hospital, but if you do have to go there, knowing your rights and responsibilities can help ensure your hospital stay is a safe and healing one.
Variations in Quality Medical and Safety of Health Care Driven by 'Perverse Incentives'
One in four patients in a hospital is harmed in some way from a medical mistake, according to the New England Journal of Medicine. Many doctors have been concerned about the quality and mistakes in healthcare, but the culture has been such that it dissuaded open discussion and transparency.
“We’re really at a very exciting time in medicine,” Dr. Makary says. “For the first time, we’re speaking up openly and honestly about this problem. We’ve got research now that supports it.
...[W]hen I was at a major medical conference once, I heard a surgeon at the podium ask the audience of thousands of doctors, 'Do you know of somebody out there in practice who should not be practicing because they are too dangerous?' And every single hand went up. Everybody seems to know about this problem. Everybody even knows of somebody who’s too dangerous to be in practice. Yet for a long time, we haven’t been honest about the problem.”Dr. Makary goes on to tell a story from his days as a medical student. A young man came to the emergency room with a fractured humerus, and the doctor told him he needed an MRI, an X-ray, and a CAT scan. The young man replied he didn’t have health insurance, at which point the doctor suddenly changed his tune, telling him to just stay off his arm, wear a sling, and all would be fine.
“I thought about it,” Dr. Makary says, “The doctor was right; all those tests don’t really change what we do, because the treatment for that type of fracture was just a sling and to rest it. So, we see these wide variations on what we do. And when you ask the doctors, 'Look, what’s going on? Why do we have so much variation in quality and safety in America?' they point out things like 'Look at our perverse incentives that promote bad care among as subgroup of doctors out there.'”
Is Your Surgery to Satisfy Your Doctor’s Quota?
Doctors are under tremendous pressure these days. Not only are they asked to see more patients per hour, many surgeons even have surgery quotas to meet.
“They’re told they need to do so many operations in a month,” Dr. Makary says. “Sometimes doctors tell me they get text messages and emails, saying, 'You need to do so many operations by the end of the month.' They’re expected to do more, often with less resources.”Quotas aren’t the only symptom of a major disconnect between healing a patient’s problem and running a for-profit disease management scheme. As discussed by Dr. Makary, sometimes a computer software program will order tests and studies automatically, and the doctor just has to sign off on them.
“Doctors don’t like blind triggers that result in overtreatment. They want to practice medicine the way it was intended to be practiced – individualized in care,” he says.While computers can help with some standardization in medicine increasing dependence on computerized diagnosis and even treatment is an issue that needs to be seriously considered and discussed. We’ve had a continually evolving improvement in artificial intelligence, so much so that in the next 20 to 30 years computers will be able to interview a patient and then spit out an entire battery of recommendations. However, the recommendations will only be as good as the information it’s based on. What good will it do if all RoboDoc can do is spit out tests and treatment protocols based on biased, inaccurate or fraudulent data at a more efficient rate than human M.D.'s?
Unnecessary Treatment is a Massive Problem
According to a report by the Institute of Medicine, an estimated 30 percent of all medical procedures, tests and medications may in fact be unnecessary2 – at a cost of at least $750 billion a year3 (plus the cost of emotional suffering and related complications and even death – which are impossible to put numbers on). While overuse and misuse have become a deeply ingrained part of the culture of medicine, there are hopeful signs that things are starting to change. Dr. Makary points out a number of standard blanket recommendations that have been changed in recent years, such as daily aspirin regimen, PSA testing, and annual mammograms.
“[N]ow people are saying, 'Wait a minute, maybe we’ve gone too far.' ...We told everybody for decades [that] everybody should be on an aspirin once a day. And a lot of people were saying, 'Wait a minute, do I really need to be taking a pill every day, even thought I’m totally healthy?' There were studies, and they looked at certain outcomes but a recent large study has shown that the internal bleeding consequence balances out the benefits to your heart. So we’re now pulling back that recommendation. If you have a healthy heart, if you don’t have a history of heart problems, we’re now pulling that recommendation back.
Same thing with PSA testing. You’re seeing the medical community say, 'Wait a minute, we don’t need to do a PSA test for prostate cancer on every older man in the world.' We’re also seeing the recommendations on breast cancer screening with mammography in that middle-aged group being pulled back.
We’re seeing a lot of research coming out now that’s saying some of these giant recommendations to do more stuff probably were not based on sound science. When we look at the full gamut of consequences of overtesting, we may be creating too many false-positives and hurting more people then we’re helping.”
More Doctors Beginning to Realize What They Were Taught is Wrong
Many doctors are now beginning to accept that some things they were taught in medical school is simply wrong.
“I was taught, for example, that everybody has one million nephrons (the unit in a kidney). We now know that’s not true. We now know that it ranges from 200,000 to two million, and everyone’s different. If you have a lot, you may have more of a reserve. If you have few, you may be more frail in your ability to withstand an insult to your kidney.
We were taught fat was bad for you. We were taught, 'Don’t eat fat. Fat is bad. Go low-fat everything.' That was probably wrong advice that the medical community gave to the general public. We now know that what’s far more important than avoiding fat is limiting sugar, a highly addictive substance, which a driver of obesity and heart disease and has many detrimental effects, mainly the hormonal effect of changing your fat storage balance. Little did we doctors know that by demonizing fat we were encouraging high-carbohydrate foods because they are notoriously 'low-fat.' Obesity surged parallel to the 'avoid fat' era of medicine. We are now dealing with a generation addicted to sugar and we’re seeing the largest growth in obesity in the history of the country.
In terms of the percent of our population on disability and the average time on disability, we are now the most disabled country in the world. And one leading driver is obesity-related chronic diseases—a problem burdening our healthcare system. These are lifestyle diseases (medical problems that can be avoided with better behavior). We’re now recognizing that some of the emphasis in the direction that we had in medical school was just not based on the solid evidence that we’re now seeing.”
Helping Patients and Doctors Choose Wisely
For the past two years, the American Board of Internal Medicine Foundation, one of the largest physician organizations in the US, has released reports on the most overused tests and treatments that provide limited or no benefit to the patient, or worse, causes more harm than good. Last year’s report warned doctors against using 45 tests, procedures and treatments. This year, another 90 tests and treatments were added to the list. To learn more, I encourage you to browse through the Choosing Wisely web site,4 as they provide informative reports on a wide variety of medical specialties, tests, and procedures that may not be in your best interest. As reported by NPR:5
“The idea is to curb unnecessary, wasteful and often harmful care, its sponsors say — not to ration care. As one foundation official pointed out last year, rationing is denial of care that patients need, while the Choosing Wisely campaign aims to reduce care that has no value.”Unfortunately, it seems matters will only get worse with the passage of the Affordable Care Act because it’s just a continuation of the same broken process. I agree that people should be covered under health insurance, but they should be covered with appropriate care; not care that perpetuates the same problems addressed in Dr. Makary’s book.
“What we’ve got to do is educate the everyday patient to empower themselves, to understand what they’re having done, and to learn to ask the right questions,” he says. “We’ve put together a list of sort of important questions a patient should ask, and we’ve put it on the book website, UnaccountableBook.com.
Things like: 'Do I really need to have this done? What if I don’t take this medication? And then, whatever that consequence could be, what are the odds that that could happen? And if it does happen, can we treat it once that happens?'
I remember consenting people for surgery as a resident. I was way over my head. They would ask me, 'What happens if I don’t have an operation or take a medicine?' And I just give them a standard answer sometimes. 'You could die. Something could go wrong.' And yet, I was rushing. You’re working sometimes for 40 straight hours; you’re working 120 hours a week. As a resident, you’ve got a mission. You get certain things done to get through this little list of things you need to do during the day... Research now shows that most patients are under-informed about the risks of medical tests, procedures and medications, and the benefits are overstated.”
On Referrals, and...
According to Dr. Makary, under-referral is another major issue that leads to improper medical treatment. Some doctors will simply declare that “nothing can be done,” without realizing a specialist may have an entirely different set of tools at their disposal. There are even “micro-specialists” out there specializing in a tiny area within a particular field of medicine. The trick is to find them.
“There are probably not enough referrals to specialists as there should be. I think sometimes you need to take things in your own hand and just ask for one. Or say, you know, 'Would it help if I spoke with someone who specializes in this?' Or go to their websites and find the experts. There are some very good websites out there now for patients, [like] ConsumerReportHealth.org. Medicare is now putting a lot of hospital performance up on the web in their website Hospital Compare. It’s HospitalCompare.hhs.gov. So, there are some good resources out there now.”Dr. Makary suggests asking an emergency room nurse for their recommendations for specialists and doctors well-versed in a particular ailment. Another helpful strategy can be to ask around for alternative practitioners or treatment options. Your local health food store can be a good place to start.
“If you don’t know of a nurse, secretary, doctor, or technician that works for a hospital that can give you this scoop on who’s really good, ask some of these important questions.”Dr. Makary suggests “For surgery, ask the following questions:
- Do I really need this done?
- When am I going to be back to feeling good?
- What if I don’t have this procedure done?
- Can I wait a year and see if this gets better?
- What if I wait and then something develops in the interim? How do we handle it that at that point and what are the odds of success then versus now?
There’s a movement – a revolution – that we described in the book Unaccountable, which is starting to provide useful information on websites, so that patients can navigate the healthcare system.”
Safeguarding Your Care While Hospitalized
Once you’re hospitalized, you’re immediately at risk for medical errors, so one of the best safeguards is to have someone there with you. Dr. Andrew Saul has written an entire book on the issue of safeguarding your health while hospitalized. Frequently, you’re going to be relatively debilitated, especially post-op when you’re under the influence of anesthesia, and you won’t have the opportunity to see the types of processes that are going on.
Dr. Makary agrees it’s important to have someone there to act as your personal advocate, or to take the time to stay with your loved one who is hospitalized. This is particularly important for pediatric patients, and the elderly.
“Sometimes, we rely on a competent talking patient to help verify what we’re doing before we go in the operating room. But if we got somebody who’s not mentally coherent because they’re elderly or a kid and there’s no family member around, these are danger zones. These are high-risk areas for medical mistakes,” Dr. Makary warns.
“It’s important to ask what procedure’s being done or why is the procedure being done. 'Can I talk to the doctor?' You have a right to know about what’s being done to you or your loved one in the hospital. When you’ve got a kid in the hospital, I think it’s particularly important to ask the questions.”For every medication given in the hospital, ask, “What is this medication? What is it for? What’s the dose?” Take notes. Ask questions. Building a relationship with the nurses can go a long way. Also, when they realize they’re going to be questioned, they’re more likely to go through that extra step of due diligence to make sure they’re getting it right—that’s human nature.
Pushing for Greater Transparency in Healthcare
The issue of transparency is a big focus of Dr. Makary’s book, Unaccountable. In it, he discusses a number of ways transparency can be improved, not only from an organization-hospital perspective, but also from an individual position perspective.
We now have a lot of data metrics to measure healthcare quality, such as different hospital’s infection rates, re-admission rates, patient satisfaction scores, and surgical complication rates. According to Dr. Makary, the ways to measure hospital performance are now maturing to the point where they need to be available to the public, and he’s seeing a “transparency revolution” starting to take place.
“I believe it’s going to reshape our entire healthcare landscape,” he says. “Instead of choosing a hospital based on a billboard advertisement or valet parking at a hospital, you should be able to look up a hospital’s performance – their quality, their volumes, and their satisfaction [rate]. You know, 60 percent of New Yorkers will look up a restaurant’s ratings before choosing a restaurant. Yet people are walking into the hospitals blind to the hospital’s performance. We’re seeing an exciting revolution now in healthcare. It’s a transparency revolution, and it’s really why I wrote this book, Unaccountable.”
Help for Victims of Preventable Medical Errors
Part of the nature of being human is that we make mistakes. No one is perfect. Mistakes will be made. And with more transparency, these mistakes will be known. So, what can you do should you find yourself a victim of a preventable medical mistake? Dr. Makary suggests connecting with patient communities like:
Besides that, he suggests:
“Ask to talk to the doctor about that mistake. If you’re not satisfied, write a letter or call the patient relations department. Every hospital is mandated to have this service. They are set up to answer your concerns. If you’re not satisfied with that, write a letter to the hospital’s lawyer, the general council. And you will see attention to the issue, because you’ve gone through the right channels.
We don’t want to encourage millions of lawsuits out there. But you know, when people voice what happened, what went wrong, and the nature of the preventable mistake, hospitals can learn from their mistakes. Sometimes they’re taking a lot of attention now to prevent mistakes from happening again. You should let that mistake be known.”
Additional Resources
Dr. Makary co-developed a checklist for surgeons to use before surgery or any other hospital procedure. His research partner, Peter Pronovost, created a checklist in the ICU for patients that are in the intensive care unit. The World Health Organization (WHO) ended up taking an interest in their checklists and used some of their principles to develop the official World Health Organization checklist.
The WHO surgical safety checklist and implementation manual,8 which is part of the campaign “Safe Surgery Saves Lives” that Drs. Makary and Pronovost were a part of, can be downloaded here. If a loved one is in the hospital, print it out and bring it with you, as this can help you protect your family member or friend from preventable errors in care. You can also learn more in Dr. Makary’s book, available on UnaccountableBook.com and other book stores.
Avoiding Unnecessary Medical Care Can Save Your Life
One of the reasons I am so passionate about sharing the information on this site about healthy eating, exercise, and stress management with you is because it can help keep you OUT of the hospital. But if you do have to go there, you need to know how to play the game.
My primary recommendation is to avoid hospitals unless it's an absolute emergency and you need life-saving medical attention. In such cases, it's advisable to bring a personal advocate -- a relative or friend who can speak up for you and ensure you're given proper care if you can't do so yourself. If you're having an elective medical procedure done, remember that this gives you greater leeway and personal choice—use it!
Many believe training hospitals will provide them with the latest and greatest care, but they can actually be far more dangerous. As a general rule, avoid elective surgeries and procedures during the month of July because this is when brand new residents begin their training. According to a 2010 report in the Journal of General Internal Medicine,9 lethal medication errors consistently spike by about 10 percent each July, particularly in teaching hospitals, due to the inexperience of new residents. Also be cautious of weekends.
Knowing how to prevent disease so you can avoid hospitals in the first place is clearly your best bet. One of the best strategies on that end is to optimize your diet. You can get up to speed on that by reviewing my comprehensive Nutrition Plan. Additionally, knowing what to do to make your hospital stay as safe as possible is equally important if you have the misfortune of being hospitalized. Understand that you, the patient, are the most powerful entity within the entire hospital system. However, the system works on the assumption that the patient will not claim that power. Knowing your rights and responsibilities can help ensure your hospital stay is a safe and healing one.
Subscribe to:
Comments (Atom)





