Misconception: Most people who have metabolic and bariatric surgery regain their weight.
Truth:
As many as 50 percent of patients may regain a small amount of weight (approximately 5 percent) two years or more following their surgery. However, longitudinal studies find that most bariatric surgery patients maintain successful weight-loss long-term. ‘Successful’ weight-loss is arbitrarily defined as weight-loss equal to or greater than 50 percent of excess body weight. Often, successful results are determined by the patient, by their perceived improvement in quality of life. In such cases, the total retained weight-loss may be more, or less, than this arbitrary definition. Such massive and sustained weight reduction with surgery is in sharp contrast to the experience most patients have previously had with non-surgical therapies.
The Real Truth:
Patients lose weight after WLS for a few months and then they figure out how to circumvent the restriction and the malabsorption of calories. Their weight loss slow and then they start packing the weight back on.
Gastric bypass which is the most effective bariatric butchery offered is not as effective as the greedy and dangerous weight loss surgery industry claims. Within the first two years of surgery, patients may lose up to 60% of their extra weight. Five years out, 85% of patients will regain more than 1/2 the weight and 15% will regain the weight they lost and then some.
Misconception: The chance of dying from metabolic and bariatric surgery is more than the chance of dying from obesity.
Truth:
As your body size increases, longevity decreases. Individuals with severe obesity have a number of life-threatening conditions that greatly increase their risk of dying, such as type 2 diabetes, hypertension and more. Data involving nearly 60,000 bariatric patients from ASMBS Bariatric Centers of Excellence database show that the risk of death within the 30 days following bariatric surgery averages 0.13 percent, or approximately one out of 1,000 patients. This rate is considerably less than most other operations, including gallbladder and hip replacement surgery. Therefore, in spite of the poor health status of bariatric patients prior to surgery, the chance of dying from the operation is exceptionally low. Large studies find that the risk of death from any cause is considerably less for bariatric patients throughout time than for individuals affected by severe obesity who have never had the surgery. In fact, the data show up to an 89 percent reduction in mortality, as well as highly significant decreases in mortality rates due to specific diseases. Cancer mortality, for instance, is reduced by 60 percent for bariatric patients. Death in association with diabetes is reduced by more than 90 percent and that from heart disease by more than 50 percent. Also, there are numerous studies that have found improvement or resolution of life-threatening obesity-related diseases following bariatric surgery. The benefits of bariatric surgery, with regard to mortality, far outweigh the risks. It is important to note that as with any serious surgical operation, the decision to have bariatric surgery should be discussed with your surgeon, family members and loved ones.
The Real Truth:
Mortality rates from weight loss surgery are far higher than the weight loss industry would have you believe. The truth is, 1 in 50 people who have gastric bypass surgery die because of it. In case you missed it, 1 in 50 people who have gastric bypass surgery DIE because of it! And that is within the first month!
Misconception: Surgery is a ‘cop-out’. To lose and maintain weight, individuals affected by severe obesity just need to go on a diet and exercise program.
Truth:
Individuals affected by severe obesity are resistant to long-term weight-loss by diet and exercise. The National Institutes of Health Experts Panel recognize that ‘long-term’ weight-loss, or in other words, the ability to ‘maintain’ weight-loss, is nearly impossible for those affected by severe obesity by any means other than metabolic and bariatric surgery. Bariatric surgeries are effective in maintaining long-term weight-loss, in part, because these procedures offset certain conditions caused by dieting that are responsible for rapid and efficient weight regain following dieting. When a person loses weight, energy expenditure (the amount of calories the body burns) is reduced. With diet, energy expenditure at rest and with activity is reduced to a greater extent than can be explained by changes in body size or composition (amount of lean and fat tissue). At the same time, appetite regulation is altered following a diet increasing hunger and the desire to eat. Therefore, there are significant biological differences between someone who has lost weight by diet and someone of the same size and body composition to that of an individual who has never lost weight. For example, the body of the individual who reduces their weight from 200 to 170 pounds burns fewer calories than the body of someone weighing 170 pounds and has never been on a diet. This means that, in order to maintain weight-loss, the person who has been on a diet will have to eat fewer calories than someone who naturally weighs the same. In contrast to diet, weight-loss following bariatric surgery does not reduce energy expenditure or the amount of calories the body burns to levels greater than predicted by changes in body weight and composition. In fact, some studies even find that certain operations even may increase energy expenditure. In addition, some bariatric procedures, unlike diet, also causes biological changes that help reduce energy intake (food, beverage). A decrease in energy intake with surgery results, in part, from anatomical changes to the stomach or gut that restrict food intake or cause malabsorption of nutrients. In addition, bariatric surgery increases the production of certain gut hormones that interact with the brain to reduce hunger, decrease appetite, and enhance satiety (feelings of fullness). In these ways, bariatric and metabolic surgery, unlike dieting, produces long-term weight-loss.
The Real Truth:
Bariatric surgery is forced bulimia. Losing weight and keeping it off is never a matter of can't and it is always a matter of WON'T. Weight loss surgery does not fix the problem. There is nothing wrong with your digestive system but there is something wrong with your brain, your behavior, and your morals. There is no nice way to put it. YOU ARE A GLUTTON! Over the years you continued to reward yourself like a trainer rewards a trained seal by tossing it a fish but in the case of the seal, the seal deserves the reward because it did something noteworthy. As a hedonistic glutton, you are rewarding yourself with glutton food that has been designed especially for you gluttons like you. You can stop eating highly flavored high-calorie junk food but you won't.
If you won't stop eating like a pig, by all means, get this surgery and please die like the pig that you are because the world would be better off without you and so would your kids.
Misconception: Many bariatric patients become alcoholics after their surgery.
Truth:
Actually, only a small percentage of bariatric patients claim to have problems with alcohol after surgery. Most (but not all) who abuse alcohol after surgery had problems with alcohol abuse at some period of time prior to surgery. Alcohol sensitivity, (particularly if alcohol is consumed during the rapid weight-loss period), is increased after bariatric surgery so that the effects of alcohol are felt with fewer drinks than before surgery. Studies also find with certain bariatric procedures (such as the gastric bypass or sleeve gastrectomy) that drinking an alcoholic beverage increases blood alcohol to levels that are considerably higher than before surgery or in comparison to the alcohol levels of individuals who have not had a bariatric procedure. For all of these reasons, bariatric patients are advised to take certain precautions regarding alcohol:
- Avoid alcoholic beverages during the rapid weight-loss period
- Be aware that even small amounts of alcohol can cause intoxication
- Avoid driving or operating heavy equipment after drinking any alcohol
- Seek help if drinking becomes a problem
If you feel the consumption of alcohol may be an issue for you after surgery, please contact your primary care physician or bariatric surgeon and discuss this further. They will be able to help you identify resources available to address any alcohol-related issues.
The Real Truth:
Alcoholic abuse happens because of weight loss surgery.
The researchers followed more than 2,000 patients who had weight-loss surgery at 10 hospitals across the United States.
Over seven years, more than 1 in 5 who had Roux-en-Y gastric bypass weight-loss surgery developed a problem such as alcohol abuse or alcoholism, compared with around 11 percent of those who underwent gastric banding.
Misconception: Surgery increases the risk for suicide.
Truth:
Individuals affected by severe obesity who are seeking bariatric and metabolic surgery are more likely to suffer from depression or anxiety and to have lower self-esteem and overall quality of life than someone who is normal weight. Bariatric surgery results in highly significant improvement in psychosocial well-being for the majority of patients. However, there remain a few patients with undiagnosed preexisting psychological disorders and still others with overwhelming life stressors who commit suicide after bariatric surgery. Two large studies have found a small but significant increase in suicide occurrence following bariatric surgery. For this reason, comprehensive bariatric programs require psychological evaluations prior to surgery and many have behavioral therapists available for patient consultations after surgery.
The Real Truth:
The truth is people who get gastric bypass surgery are 4 times more likely to kill themselves than people who don't get it. If the above industry bullshit were true and if gastric bypass were to increase the patient's self-esteem and their quality of life, they would be less likely to kill themselves rather than be more likely.
The next lie in the above industry bullshit " comprehensive bariatric programs require psychological evaluations prior to surgery and many have behavioral therapists available for patient consultations after surgery" proves my point. If they have improved self-esteem, higher quality life, and are receiving professional counseling to boot then their reasons for committing suicide would be far lower than that of the general population but instead, it is much much higher.
I can only speculate as to why. I suspect that a lot of why bariatic surgery victims kill themselves is because of the painful complications caused by weight loss surgery. In addition to that, they are no longer to pleasure themselves with food because eating becomes very painful for some gastric surgery victims and since most fat people live to eat rather than eat to live and their lives revolve around food. Food is their life.
There is also the malabsorption factor. Gastric bypass victims are unable to absorb the nutrients that are essential for good physical and mental health.
Misconception: Bariatric patients have serious health problems caused by vitamin and mineral deficiencies.
Truth:
Bariatric operations can lead to deficiencies in vitamins and minerals by reducing nutrient intake or by causing reduced absorption from the intestine. Bariatric operations vary in the extent of malabsorption they may cause, and vary in which nutrients may be affected. The more malabsorptive bariatric procedures also increase the risk for protein deficiency. Deficiencies in micronutrients (vitamin and minerals) and protein can adversely affect health, causing fatigue, anemia, bone and muscle loss, impaired night vision, low immunity, loss of appropriate nerve function and even cognitive defects. Fortunately, nutrient deficiencies following surgery can be avoided with appropriate diet and the use of dietary supplements, i.e. vitamins, minerals, and, in some cases, protein supplements. Nutrient guidelines for different types of bariatric surgery procedures have been established by the ASMBS Nutritional Experts Committee and published in the journal, Surgery for Obesity and Other Related Disorders. Before and after surgery, patients are advised of their dietary and supplement needs and followed by a nutritionist with bariatric expertise. Most bariatric programs also require patients to have their vitamins and minerals checked on a regular basis following surgery. Nutrient deficiencies and any associated health issues are preventable with patient monitoring and patient compliance in following dietary and supplement (vitamin and mineral) recommendations. Health problems due to deficiencies usually occur in patients who do not regularly follow-up with their surgeon to establish healthy nutrient levels.
The Real Truth:
Nutrient deficiencies are unavoidable after gastric bypass and other weight loss surgery. Correcting them is hit and miss at best. The industry attempts to blame the patient/victim but the reasons they are not absorbing nutrients are:
1. Dumping syndrome: As soon as the food is eaten it rapidly goes from the mouth to the anus and then in the patient's underwear or toilet so nutritional content doesn't have time to get absorbed.
2. The stomach no longer works correctly: The function of the stomach is to prepare the food for absorption of the small intestine. After the stomach is turned into a "pouch" it can no longer do its job so when the food reaches the small intestines it nutrient content cannot be extracted.
3: Most of the small intestine is bypassed: A normal small intestine is 20 feet long. It has to be that long in order to absorb the essential nutrients humans need. After gastric bypass surgery there is not enough small intestine left to do its job of absorbing nutrients.
Misconception: Obesity is only an addiction, similar to alcoholism or drug dependency.
Truth:
Although there is a very small percentage of individuals affected by obesity who have eating disorders, such as binge eating disorder syndrome, that may result in the intake of excess food (calories), for the vast majority of individuals affected by obesity, obesity is a complex disease caused by many factors. When treating addiction, such as alcohol and drugs, one of the first steps is abstaining from the drugs or alcohol. This approach does not work with obesity as we need to eat to live. Additionally, there may be other issues affecting an individual’s weight, such as psychological issues. Weight gain generally occurs when there is an energy imbalance or, in other words, the amount of food (energy) consumed is greater than the number of calories burned (energy expended) by the body in the performance of biological functions, daily activities and exercise. Energy imbalance may be caused by overeating or by not getting enough physical activity and exercise. There are other conditions, however, that affect energy balance and/or fat metabolism that do not involve excessive eating or sedentary behavior including:
- Chronic sleep loss
- Consumption of foods that, independent of caloric content, cause metabolic/hormonal changes that may increase body fat (sugar, high fructose corn syrup, trans fat, processed meats and processed grains)
- Low intake of fat-fighting foods (fruits, vegetables, legumes, nuts, seeds, quality protein)
- Stress and psychological distress
- Many types of medications
- Pollutants
Obesity also ‘begets’ obesity, which is one of the reasons why the disease is considered ”progressive.” Weight gain causes a number of hormonal, metabolic and molecular changes in the body that increase the risk for even greater fat accumulation and obesity. Such obesity-associated changes reduce fat utilization, increase the conversion of sugar to fat, and enhance the body’s capacity to store fat by increasing fat cells size and numbers and by reducing fat breakdown. Such defects in fat metabolism mean that more of the calories consumed are stored as fat. To make matters worse, obesity affects certain regulators of appetite and hunger in a manner that can cause an increase in the amount of food eaten at any given meal and the desire to eat more often. There are many causes for obesity and that the disease of obesity is far more than just an ‘addiction’ toward food. The treatment of obesity solely as an addiction may be beneficial for a very small percentage of individuals whose only underlying cause for obesity is excessive and addictive eating, but would be unlikely to benefit the multitudes, particularly those individuals affected by severe obesity.
The Real Truth:
Obesity is multifactorial but it is not a disease. It is a complex disorder of a moral, psychological, cultural, societal and organic nature. It is not a disease!
In the1970s the obesity rate in the US was 3%. Today, it is 36% and in the gluttonous and immoral red states, it is even higher. To say that gluttony is a disease is like saying, greed, lust, jealousy, sloth, avarice, pride are also diseases.
The cause of obesity is gluttony. Doctors will lie and deny this but the only way one can get fat is to eat too much. Fat people CHOOSE to eat too much and they CHOOSE to do it too much of the time. That is gluttony. If they were not weak willed gluttons with a weak sense of personal and societal responsibility they would stop their chronic and repulsive overeating. They fail to do so. This goes to the moral part of the equation.
They are told by the worthless diet industry that being a fat ass is their fault. The industry has convinced them that there is some sort of weight loss magic that will cause them to lose weight with almost no effort. Many of them are convinced that they have some mysterious metabolic disorder that causes their metabolic rates to be impossibly slow. A lot of them simply lie and say they barely eat. This is a moral and psychological part of the equation.
American culture is food-centric. Everything we do has become an excuse to have a feast. Americans are also quite uncouth and the lower their IQs and the further to the right on the political spectrum they are the fatter and more uncouth they become. This goes to culture and society.
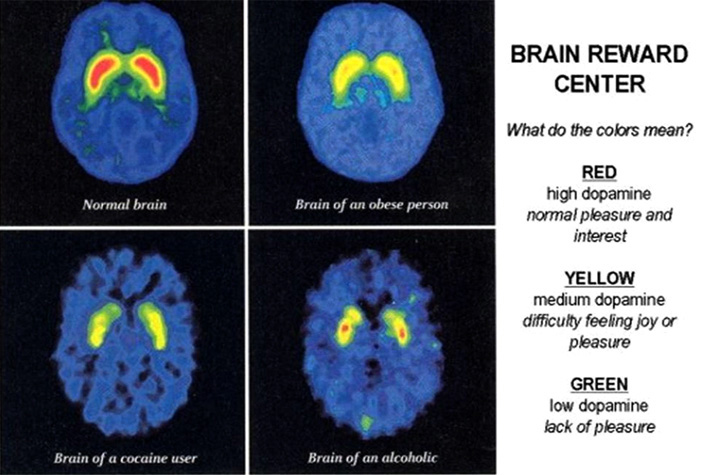
The organic part is more complex because it goes to addiction. The brain of a glutton looks a lot like the brain scan of a drunk or a coke head. The brains of gluttons, drunks and coke heads don't start out abnormal. They become abnormal due to chronic substance abuse. A glutton is not an addict like in the case of the coke head. The glutton is a more like the drunk in that the glutton is a substance abuser, like the drunk, CHOOSES to lie and then deny the nature of the problem.
If the coke head, drunk or glutton screwed up their courage and stopped acting like a spoiled brat and stopped the coke, drinking, and gormandizing their brains would return to normal but sadly most of them lack the moral or psychological fortitude to stop so they don't.
The immediate answer for the boozing, snorting, and gluttony is harsh shaming and unrelenting ridicule. AKA tough love.